Top 5 Mechanical Running Faults
In my last post we discussed some running gait pattern norms. Once again, it is difficult to completely standardize running gait however researchers have been able to set a range of “optimal” angles and loads through extensive observation on runners with and without pain. So now we know that anything deviates TOO MUCH from the closest thing to a standard can produce future problems. For clinicians who want to analyze gait a few recommendation for you would be: educate yourself on running gait normal and abnormal patterns, and strongly consider observing running gait in slow motion or use some of gait analysis system. It is really difficult to see under the naked eye unless you have observed thousands of runners and actually paid attention to mechanics.
Recall what I stated in the first post, “in order to run the athlete has be able to properly absorb shock, demonstrates proper alignment of the lower quarter joint and demonstrates good stability of the trunk, pelvis, knee, and ankle”. Or as I put it “YOU HAVE TO BE FIT TO RUN.”
When analyzing running gait, crucial deviation or faults will be seen during initial contact through all the way through toe off (the period of time one foot is on the ground). With that being said, lets look at the top 5 common running mechanical deviations. This may be helpful to some runners and clinicians who are trying to figure out why the athlete may be experiencing pain.
Some of these faults can occur together. Some runners exhibit 1 or 2 deviation, some more than that. We must remember that the lower quarter is connected chain. What happens at the hip can affect the knee and foot and vice versa. If there is a weak link at either the hip or foot, or both, I can bet money that you may see some faulty movement especially the longer the run (because fatigue will settle in).
Powers et al- lecture 2018- Movement Performance Institure
1. Limited Knee Flexion During Max Loading
During the mid support phase of running gait you ideally want to observe 30-40 degrees of knee flexion. Power et al. observe that in runners that demonstrates <30 degrees of knee flexion (running on a straight knee) reported knee pain and ground reaction forces resulted to be much higher than seen in runners that demonstrates >30 degrees knee flexion.
Landing on a flexed knee helps absorb the weight of the body hitting the ground, the straighter the knee the harder the landing the less absorption by the knee and hip take place.
Why does this happen? First thing you may need to address is possible quadriceps weakness! In order for the knee to flex during loading the quadriceps needs sufficient ECCENTRIC strength.
2. The Hip Drop
I analyze running gait every day during my runs, and this is one of the most common things I see, especially in females more so than males. Ideally you don’t want to see much hip drop. The peak amount of drop desired ranges from 5-10 degrees (4). If you can see a hip drop with the naked eye- that already is too much of a hip drop. The problem with the hip drop is that since the lower limb works as a whole unit- hip drop promotes medial knee collapse and sometimes increase midfoot pronation. Many studies have shown that the runners that exhibit patellofemoral joint pain tend to demonstrate larger amounts of hip drop. Excessive hip drop contributes to spikes in knee joint compression, low back joint compression, and increase back paraspinal activity.
Therefore runners who display a hip drop may complain of back back, knee pain, hip pain, shin splints, or ITB pain.
Causes:
· weak Gluteus Medius and Maximus. Your glute maximus is the only triplanar muscle, meaning: it helps extend your thigh, bring your thigh out to the side, and externally rotate your thigh.
· ITB stiffness : can pull your thigh inward and promote hip drop.
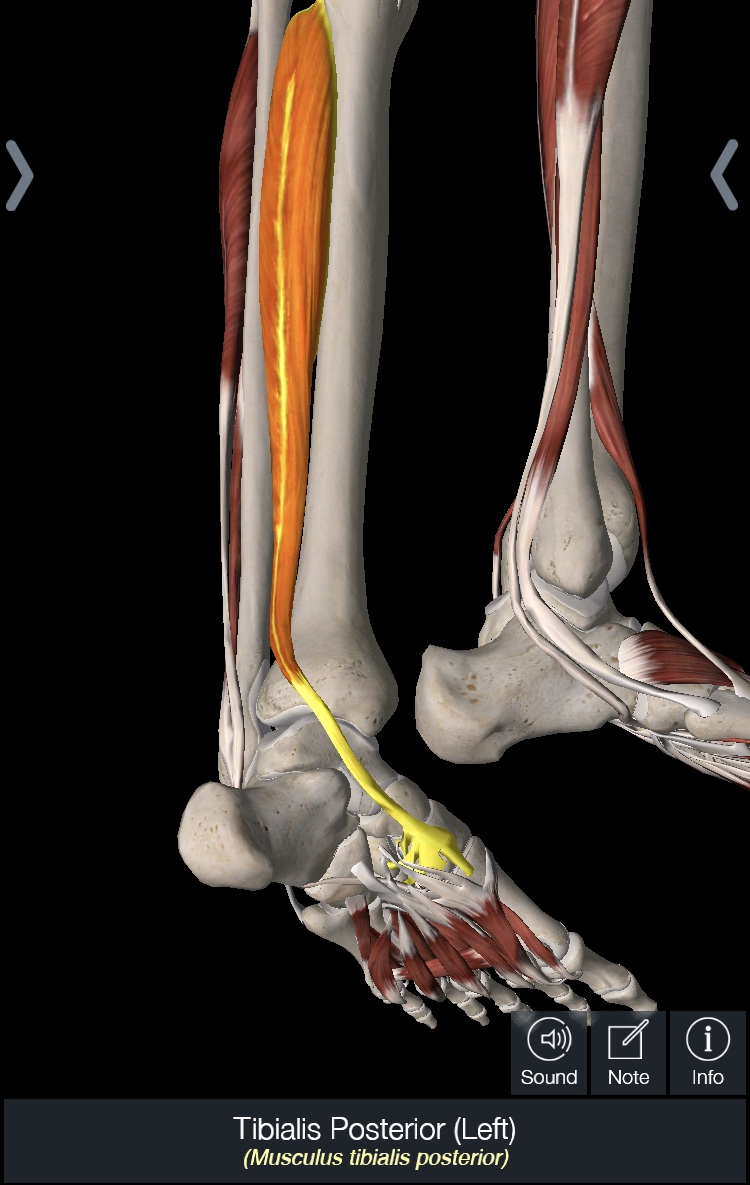
· Posterior tibialis weakness ( the foot can affect the hip remember)
How to correct:
· Strengthen your glutes!
· Gait retraining, run in front of mirror and don’t allow your hip to drop (3,6).
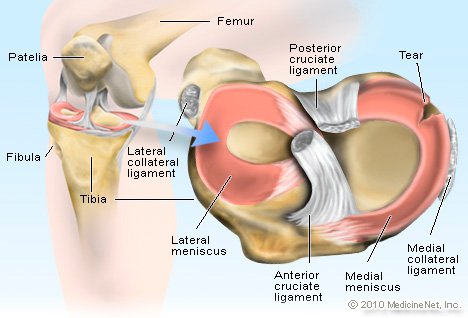
3. Knee Valgus
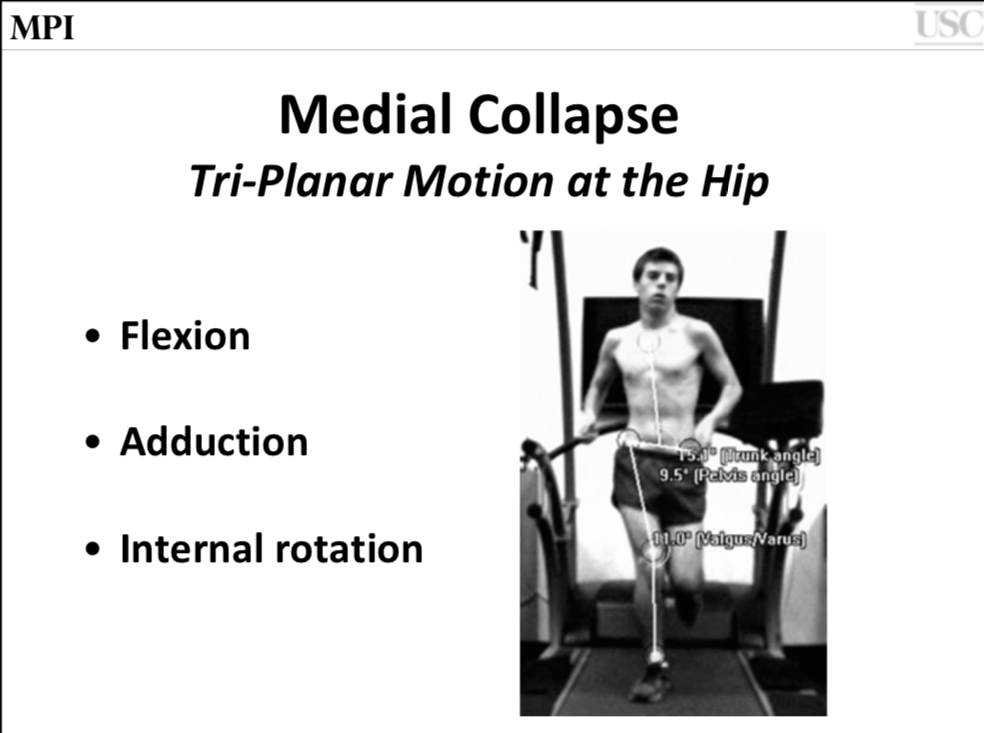
Chris Powers lecture 2018- Movement Performance Institute
Like I mentioned above the hip does affect the knee. When the pelvis drops it does shift the center of mass more towards the center causing excessive internal rotation of the thigh (2) thus creating a knee valgus angle. Since it tends to be common that the glutes will test out as weak, of course the compensation has to come from somewhere, and so therefore the quads become very dominant.
The movement impairment of the knee valgus associated with the pelvic drop and over dominant quadriceps is what commonly causes knee pain, or the commonly heard diagnoses’ of: patellofemoral joint pain syndrome, and patellar tendinitis/runners knee.
Causes:
· Weak hip external rotators and abductors (GLUTES)
· Sometimes some runners may have relatively strong glutes but may be just have a coordination problem. I have had some runners practice in front of the mirror and have them try to NOT let their knees drive in and they can correct it just by paying attention.
Correction:
· work on glute strengthening, ( clam, sidelying hip abduction, sidesteps) and pay attention to avoiding the knee from diving in.
4. Foot pronation
Loading phase:
Right foot: midfoot pronated and foot externally rotated, vs the left foot . History of posterior tibialis tendonitis on the Right Foot.
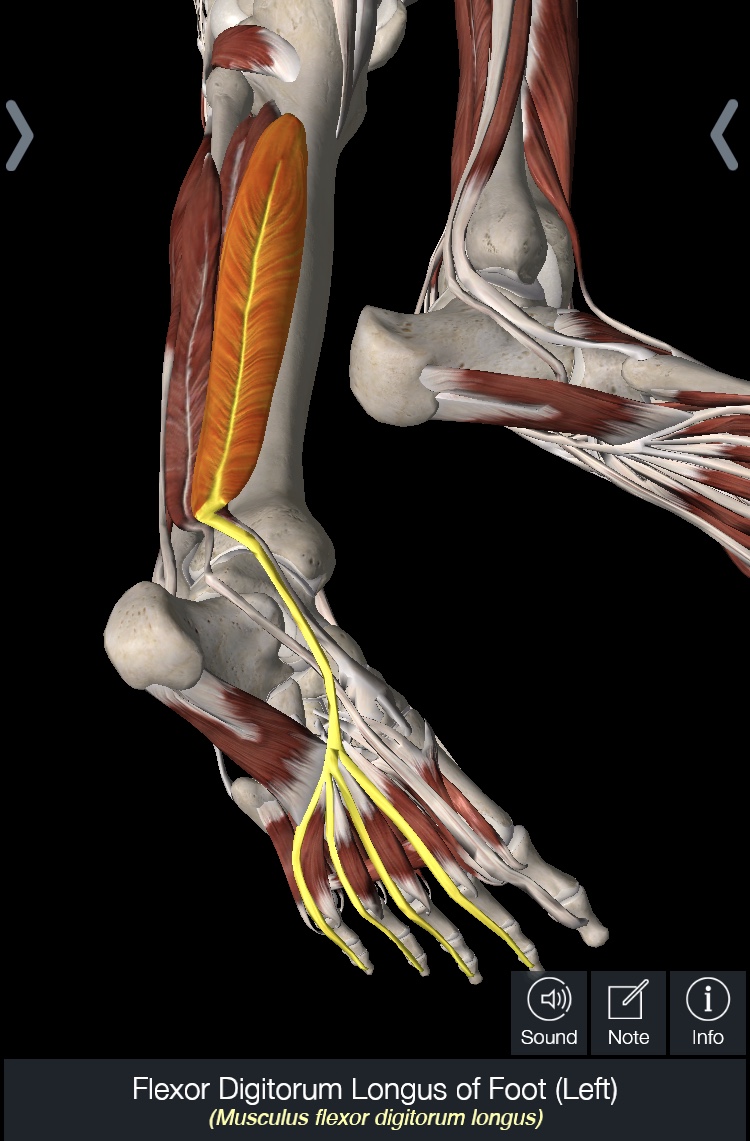
Foot pronation is when the midfoot drops towards the ground especially during the loading phases. The foot is meant to be strong but also flexible, therefore some degree of midfoot pronation is expected, however the problem is when there is an excessive amount of midfoot pronation. The peak amount of pronation desired during the loading phase of running gait is 10-15 degrees (1). Some researchers state that shoes provoke an increase in pronation, while others solely believe that weakness is the main factor, and many others believe it is more multifactorial.
This means that foot pronation can be caused by :
· stiffness of the ankle causing compensation via midfoot pronation in order to get the foot to roll over the forefoot
· pelvic drop causes a kinetic chain fault, forcing lower leg ( tibia) to externally rotate and therefore cause the midfoot to drop.
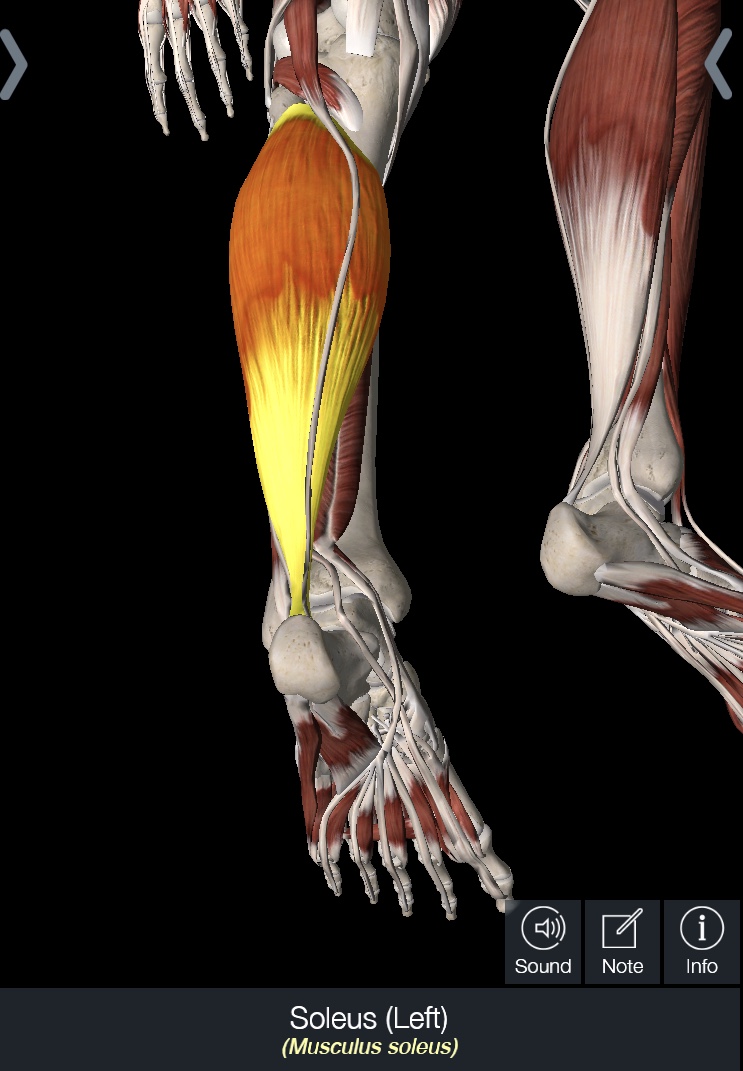
· weakness of the tibialis posterior, which helps support the midfoot.
Correction:
· correct the hip drop if you exhibit one
· Make sure you have full ankle mobility : 20 deg of ankle dorsiflexion
· Work on posterior tibialis strengthening exercises ( see previous blog for exercise tips) and try to push off big toe versus outside of foot.
5. Erect posture
Ever notice some knee or back soreness after a long or even fast run? Well you may be running with your trunk a little to stiff and straight. When you don’t slightly bend forward , you change the center of gravity back towards your hips and therefore force your body refrains from using the glutes and instead recruits the quadricep. This leads to lack of the needed TRIPLE EXTENSION during toe off. Triple extension is when the ankle pushes off, knee and hip extends via their associated extensor musles. In a study by Powers et al, researchers found that a trunk lean of 10 degrees led to a reduction in the peak patellofemoral joint stress by 13% (5).
Causes:
· Calf weakness
· Tight hip flexors- can cause and anterior pelvic tilt, so to avoid flexing your hips too much, some runners will stay up tall.
· Glute weakness
Correction:
· Try to lean forward SLIGHTLY when you are running, pick a recovery/slow run when you first attempt this.
· Strengthen core , glutes, and gastrocs
· Stretch your hips.
Quick 2 cents: Runners there is a saying, “if it aint broke dont fix it” , HOWEVER OPTIMIZING movements, strength, and mobility is BENEFICIAL!
TRAIN SMART AND RUN WELL.
Jessica Mena PT, DPT, OCS, CSCS
Doctor of Physical Therapy
Board Certified Orthopaedic Clinical Specialist
RUNNER
REFERENCES
1. Byl, N., Davis. I., Heiderscheit B., Powers. C. 2013 Research Symposium- The Science of Running,2013. CPTA Nov 9-10.
2. Dierks T. A., Manal, K., Hamill J. Davis I.S. Proximal and Distal Influences on Hip and Knee Kinematics in Runners with Patellofemoral Pain During a Prolonged Run. Journal of Sports and Orthopaedic Physical Therapy. 2008 38 (8)
3. Heiserscheit, B. Gait Retrainig for Runners- In Search of Ideal. Journal of Sports and Orthopeadic Physical Therapy. 2011. 41 (12)
4. Powers, C. The Influence of Abnormal Hip Mechanics on Knee Injury: A Biomechanical Perspective. Journal of Sports and Orthopaedic Physical Therapy. 2010 40:2
5. Teng, H-L., Powers, C. Sagittal Plane Trunk Posture Influences Patellofemoral Joint Stress During Running. Journal of Sports and Orthopaedic Physical Therapy. 2014. 44 (10) 785-792
6. Nakagawas, T.H., Maciel, C.D., Serrao F.V. Trunk Biomechanics and its association with hip and knee kinematics in patients with or without patellofemoral pain. Journal of Manual Therapy. 2015 20: 189-193 www.elsevier.com/math
7. Willy, R. W.., Scholz J.P., Davis I.S. Mirror Gait Retraining for the Treatment of Patellofemoral Pain in female Runners. Clinical Biomechanics. 2012 (27) 1045-1051